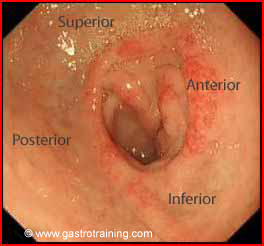
Mr Lim a 45 year old Chinese man had an endoscopy performed for epigastric pain. He was self medicating with diclofenac for toothache. Endoscopy showed:

What is the diagnosis?
Gastric ulcer- it is a discrete mucosal lesion with a punched-out smooth ulcer base. The margins are everted suggestive of a malignant ulcer
Most gastric ulcers tend to occur at the junction of the body and antrum, along the lesser curvature.
What is an ulcer?
An ulcer is a mucosal break unlike erosions which are breaks in the epithelium (i.e. ulcers are deeper)
How do you endoscopically distinguish benign from malignant ulcer?
Benign ulcers have smooth, regular and rounded edges with a flat smooth base and surrounding mucosa that shows radiating folds. The following features are suggestive of malignancy on endoscopy:
- The gastric folds around the ulcer are nodular, fused, or stop short of the ulcer margin
- The ulcers margins are irregularly heaped up or overhanging
- The ulcerated mass often protrudes into the lumen
Discuss the next steps after diagnosis of peptic ulcer?
- Exclude any stigmata of bleed like a visible vessel or an adherent clot or presence of old or recent blood in the stomach or duodenum
- Obtain biopsies from gastric ulcer to exclude malignancy. A single biopsy offers 70% accuracy in diagnosing gastric cancer, but 7 biopsy samples obtained from the base and ulcer margins increase the sensitivity to 99%.
- Stop NSAIDS, aspirin if possible
- Arrange a repeat endoscopy in 6-8 weeks to assess gastric ulcer healing
Discuss the common causes of peptic ulcer disease (PUD)?
The two main causes of PUD are HP infection and NSAIDS. Other causes:
- 15% of peptic ulcers are idiopathic or due to rare causes (rare causes -drugs like Sirolimus, gastrinoma, systemic mastocytosis, carcinoid syndrome, ischaemia, radiation injury, sarcoidosis, Crohn’s disease etc).
- COPD and cirrhosis is associated with an increased risk of PUD.
- Alcohol is not a risk factor for peptic ulcer.
- Steroids alone are not associated with an increase in the risk for peptic ulcer. However, steroids may worsen NSAID-induced ulceration.
What are the Clinical manifestations of peptic ulcer disease?
Epigastric discomfort- Classic pain of duodenal ulcer occurs in empty stomach whereas gastric ulcer (GU) causes more severe pain occurring soon after meals.
Discuss endoscopic follow-up after peptic ulcer treatment?
- Duodenal ulcers — Patients with uncomplicated DU do not need further endoscopy unless symptoms persist or recur. HP eradication should be confirmed.
- Gastric ulcers- Repeat endoscopy to confirm GU healing is the standard practice to ensure that the lesions are benign. However, a case can be made against the practice, if the initial biopsies are adequate (at least four good biopsies from the ulcer margin and one from the base).
Discuss the pharmacotherapy in bleeding peptic ulcer?
Patients with high risk stigmata (such as a visible vessel or adherent clots) are at high risk of rebleeding. 80 mg bolus (of omeprazole or pantoprazole) followed by 8 mg/hr infusion has become the standard in clinical practice after endoscopic treatment of the ulcer. If there is no rebleeding within 24 hours, the patient may be switched to oral pantoprazole 40 mg/day or omeprazole 20 mg/day. Twice daily dosing of an oral or IV proton pump inhibitor may also be a reasonable alternative.
Discuss the role of primary prophylaxis for peptic ulcer?
The American College of Gastroenterology has identified the five most important variables that place patients at risk for NSAID-related gastrointestinal complications:
- Prior history of a gastrointestinal event (ulcer, haemorrhage)
- Age >60
- High dosage of a NSAID
- Concurrent use of glucocorticoids
- Concurrent use of anticoagulants
Patients with these risk factors should be considered for prophylaxis with NSAID treatment
What are the modes of ulcer prevention i.e. prophylactic treatment?
HP eradication with NSAIDs: is of value; however PPI maintenance is better in preventing ulcer recurrence and/or bleeding with NSAIDs.
However, patients receiving long term PPI treatment for prevention of NSAID ulcers should be tested for H pylori to reduce the PPI-H pylori interaction leading to accelerated loss of specialised glands and atrophic gastritis.
HP eradication with aspirin: HP eradication is equivalent to PPI treatment in preventing further bleeds if aspirin is continued. Eradication followed by PPI maintenance after aspirin bleed reduces the risk even further (almost cures the problem).
Bottom line – Always eradicate H. Pylori and use PPI prophylaxis in patients with complicated ulcer disease.
Discuss the endoscopic description of duodenal ulcer?
More than 95% of the duodenal ulcers occur in the first part of the duodenum. It has four walls described endoscopically as anterior, posterior, superior and inferior.
Further reading






