Mr Jacques, a 60 year old investment banker presented with complaints of dyspepsia and weight loss of a stone over the last 10 weeks. Endoscopy showed:
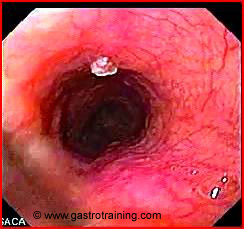
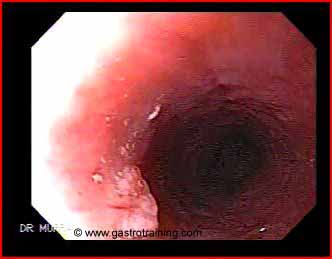
What is the diagnosis?
A small mucosal lesion is seen- it is a squamous cell papilloma
It is an incidental finding and not responsible for the patient’s symptoms.

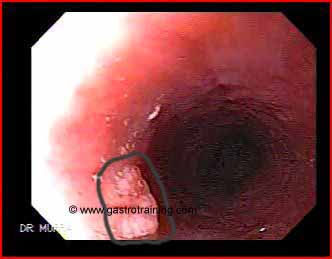
Discuss the endoscopic findings of a squamous cell papilloma?
Squamous cell papilloma is a pinkish soft polypoid structure with a smooth or slightly rough surface in the oesophagus. They are usually 5-6 mm in size but could be large. The most frequent location is the posterior wall of the lower third of the oesophagus, and the lesions are usually isolated.
Discuss the aetiology of a squamous cell papilloma?
Oesophageal Squamous papilloma is rare; with an estimated prevalence of 0.01 to 0.43. The aetiology of squamous cell papilloma is unclear. Theories:
Viral infection by human papilloma virus has also been implicated.
Hyper-regenerative response of the mucosa to chemical and mechanical irritation such as minor trauma, previous gastroesophageal surgery and GORD.
Discuss the clinical manifestations of squamous cell papilloma?
Oesophageal squamous papilloma is mostly asymptomatic and the lesion is incidentally discovered at endoscopy. A large papilloma can sometimes cause dysphagia.
Discuss the malignant potential of squamous cell papilloma?
There are no reports of malignant transformation in humans. However, there is debate about its malignant potential in human because HPV DNA has been isolated from oesophageal cancer, papilloma is known to be precursor of squamous carcinoma (as in larynx and cervix), and papilloma and occult epidermoid carcinoma of oesophagus have been found contiguously in humans. There is also evidence for oesophageal squamous papillomas in cows that undergo malignant transformation after exposure to specific environmental carcinogens .Therefore malignant transformation still remains a concern.
Discuss the management of squamous cell papilloma?
All oesophageal squamous papillomas should be removed both for diagnosis and secondary to the ambiguity at present about malignant potential.
They are easily removed, with forceps (if small) or snare polypectomy (with or without EMR)
Image courtesy of www.gastrointestinalatlas.com






