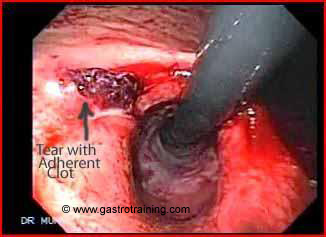
Oesophageal module Mrs Patterson, a 26 year old housewife was admitted to the hospital with an episode of haematemesis following an alcoholic binge. Her endoscopy showed:

What is the diagnosis? Mallory -Weiss Tear (MWT)
What is Mallory- Weiss syndrome?
Mallory-Weiss syndrome is characterized by longitudinal mucosal lacerations in the distal oesophagus and proximal stomach, which are usually associated with forceful retching. The lacerations often lead to bleeding from submucosal arteries.
Discuss the pathophysiology of MWT?
MWT likely occurs as a result of a large, rapidly occurring, and transient transmural pressure gradient across the region of the GO junction. Retching or vomiting causes a rapid rise in intragastric pressure causing a dramatic increase in the transmural pressure across the GO junction which abuts a low intrathoracic pressure zone. Another potential mechanism for MWTs is the violent prolapse or intussusception of the upper stomach into the oesophagus, as can be witnessed during forceful retching at endoscopy.
Discuss the clinical manifestations of MWT?
- The classic presentation consists of an episode of haematemesis following a bout of retching or vomiting. Less common presenting symptoms include melaena, haematochezia, syncope, and abdominal pain.
- Bleeding from MWTs stops spontaneously in 80-90% of patients. With conservative therapy, most tears heal uneventfully within 48 hours. Thus, a MWT can easily be missed if endoscopy is delayed.
- The degree of blood loss varies. Hemodynamic instability and shock may occur in up to 10% of patients.
Discuss the role of hiatus hernia in MWT?
Hiatus hernia has been found in 35-100 % of patients with Mallory-Weiss tears and has been considered by some to be a necessary predisposing factor. During retching or vomiting, the transmural pressure gradient is greater within the hernia than the rest of the stomach, and it is the location most likely to sustain a tear. Within the hernia, the tear is more likely to involve the lesser curvature of the gastric cardia, which is relatively immobile compared to the remainder of the stomach.
Discuss the endoscopic management of MWT?
Endoscopic diagnosis of a MWT is readily made by identifying active bleeding, an adherent clot, or a fibrin crust over a mucosal split within or near the gastroesophageal junction. The split is usually 2-3 cm in length. Most patients present with a single tear. The usual location of the tear is just below the gastroesophageal junction on the lesser curvature of the stomach (between 2 and 6 o’clock on endoscopic viewing with the patient in the left lateral decubitus position). Patients with active bleeding are treated. Stigmata (e.g., nonbleeding visible vessel, adherent clot) do not necessarily require treatment in MWTs as they do in peptic ulcers as the risk of rebleeding is very low. Such stigmata usually are not treated unless they are rebleeding episodes from the same lesion or are associated with a coagulopathy. Some experts will treat a non bleeding visible vessel. Actively bleeding lesions can be treated with adrenaline injection and haemoclips or contact thermal methods as in peptic ulcer bleeds. Band ligation is also an efficient procedure for primary haemostasis and for preventing recurrent bleeding. Angiography (gelfoam embolization of the left gastric artery) or surgery may be needed if endoscopy fails to control to bleeding.
Discuss the role of PPI in MWT?PPI’s are usually prescribed for 1-2 weeks to accelerate healing, although this practice is of unproven benefit. An antiemetic is useful for controlling nausea and vomiting, common precipitating factors to MWTs.
Discuss the time for safe discharge? Patients with actively bleeding MWTs should be hospitalized for at least 48 hours. Patients with clinical risk factors for rebleeding and endoscopic stigmata of nonbleeding visible vessel, pigmented protuberance, or adherent clot should be observed for 48 hours. If rebleeding occurs, it usually takes place within that time period.
Other patients can be discharged after observation for approximately 24 hours.
Image courtesy of www.gastrointestionalatlas.com






