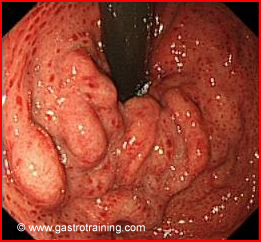
Mr Turner, a 49 year old man had an endoscopy performed for iron deficiency anaemia. It showed
What is the diagnosis?
Portal hypertensive gastropathy (PHG) with gastroesophageal varices
What is PHG?
PHG is a poorly understood complication of portal hypertension. It is defined as a condition in which macroscopic alterations occur in the gastric mucosa, which are associated with mucosal and submucosal vascular ectasia in the absence of any histological evidence of an inflammatory process.
What is the clinical significance of PHG?
- The clinical significance of this condition lies in its potential to lead to acute and chronic bleeding in patients with cirrhosis and portal hypertension.
- Generally, patients who develop PHG have more severe liver disease, and one could argue that PHG might be a marker of more severe liver disease in patients with cirrhosis.
- In PHG there is an increased susceptibility to gastric damage especially to NSAIDs.
Discuss the pathogenesis of PHG?
- Up to 65% of patients with cirrhotic portal hypertension will develop PHG, often with the presence of oesophageal and/or gastric varices. PHG can occur in non cirrhotic portal hypertension too (e.g. non cirrhotic portal fibrosis or extra hepatic portal obstruction)
- The mechanism by which patients with portal hypertension develop portal hypertensive gastropathy is unclear. Its pathogenesis is known to be multifactorial, involving elevations in portal pressure and alterations in the blood flow of the gastric mucosa and in the regulatory mechanism of local vascular tonus.
Discuss the diagnosis of PHG?
There is no gold standard diagnosis or a consensual definition for portal hypertensive gastropathy. The diagnosis of PHG is made endoscopically. In mild PHG (65-90% of cases) the gastric mucosa often looks reddened and oedematous with a snakeskin or mosaic pattern. Severe PHG is defined by cherry red spots which are typically very friable and can actively bleed during endoscopy.
In PHG, changes in the gastric mucosa are typically localised to the fundus or corpus of the stomach but PHG-like conditions have been described elsewhere in the gastrointestinal tract, including the rectum, colon, and small bowel.
Discuss the clinical manifestations of PHG?
Although patients with PHG can present with melaena, they more commonly present with chronic anaemia which can be transfusion dependent
Discuss the treatment of PHG?
- The most important pharmacotherapy for PHG involves the use of beta blockers. Propanolol reduces recurrent bleeding in PHG y reducing gastric blood flow.
- Both vasopressin and glypressin have been shown to cause a reduction in gastric blood flow but at the expense of decreasing mucosal oxygenation. Their role in the management of PHG associated bleeding has not been assessed.
- Oestrogen and progesterone have been reported anecdotally to reduce bleeding from PHG.
- TIPS or Portocaval shunts have been used as a surgical means of controlling PHG associated bleeding.
- Liver transplantation ultimately reverses portal hypertension and therefore effectively treats PHG






