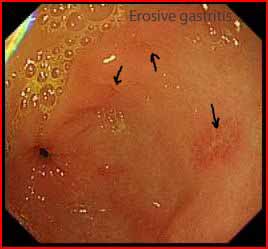
Mr Curtis, a 25 year old student presents with vomiting after an alcoholic binge. His endoscopy showed:

What is the diagnosis?
Non erosive gastritis
The picture shows mucosal erythema and oedema consistent with acute gastritis.
What is gastritis?
- Gastritis technically refers to endoscopic or histological findings of inflammatory changes in the gastric mucosa; however, the term is often used clinically to refer to the symptoms of dyspepsia.
- No correlation exists between microscopic inflammation (histologic gastritis) and the presence of gastric symptoms (e.g., abdominal pain, nausea, vomiting). In fact, most patients with histologic evidence of acute gastritis (inflammation) are asymptomatic.
- The inflammation may involve the entire stomach (pangastritis) or a region of the stomach (e.g., antral gastritis).
What are the causes of gastritis?
The mechanism of injury in gastritis is an imbalance between the aggressive and the defensive factors that maintain the integrity of the gastric mucosa. Acute gastritis can be:
Erosive gastritis: can result from the exposure to a variety of agents or factors. This is referred to as reactive gastritis. These agents/factors include aspirin, NSAIDs, alcohol, potassium, iron supplements, cocaine, stress, radiation, bile reflux, and ischemia. The gastric mucosa exhibits haemorrhages (hemorrhagic gastritis), erosions, and ulcers.
Non erosive gastritis: generally caused by H. Pylori.
What are the clinical manifestations of acute gastritis?
Acute gastritis may produce no symptoms but can be associated with short-lived dyspepsia, lack of appetite, nausea or vomiting. It can occasionally be severe enough
to cause gastrointestinal bleeding with melaena or haematemesis
Discuss the treatment of gastritis?
- Gastritis generally clears spontaneously.
- No specific therapy exists for acute gastritis, except for cases caused by H pylori.
- Discontinue the use of drugs known to cause gastritis (e.g., NSAIDs, alcohol).
Image courtesy of www.gastrointestinalatlas.com






