Obesity
How do you diagnose obesity?
The degree of overweight or obesity in adults should be defined as follows.
?
| Classification | BMI (kg/m2) |
|---|---|
| Healthy weight | 18.5–24.9 |
| Overweight | 25–29.9 |
| Obesity I | 30–34.9 |
| Obesity II | 35–39.9 |
| Obesity III | 40 or more |
Is measurement of waist circumference important?
Health risks of obesity are independently associated with abdominal fat measured by waist circumference. Thus, health risks are increased with increased waist circumference.
| BMI classification | Waist circumference | |||
|---|---|---|---|---|
| low | High | Very high | ||
| Men | < 94 cm | 94–102cm | >102cm | |
| Women | < 80 cm | 80–88cm | >88cm | |
| Overweight | No increased risk | Increased risk | High risk | |
| Obesity I | Increased risk | High risk | Very high risk | |
Why treat obesity?
- Co-morbidities
- Life style
- Improved survival
Obesity is associated with multiple co-morbidities
- Endocrine- Diabetes
- Cardiovascular- hypertension, hyperlipidemia, coronary & cerebral vascular disease
- Gynaecology- infertility and menstrual irregularities
- Orthopaedic- arthralgia, low back pain
- Dermatology- fungal infections
- Pulmonary- sleep apnea, asthma, pulmonary hypertension, hypoventilation
- GI- GORD, cholelithiasis, fatty liver/liver dysfunction
- Socio economic- discrimination
- Psychological- depression
- Increased risk of cancers
What is the health risks associated with obesity?
Obesity is second only to smoking as the leading cause of preventable death in the US.
More than 110,000 deaths/year in the US are associated with obesity.
Are any tests needed before treating obesity?
No single laboratory test is indicated for all patients with obesity. The specific evaluations will depend on presentation of symptoms, risk factors, and index of suspicion.
- Screen for co-morbidities- so check blood glucose, and lipids. Check for hypertension, obstructive sleep apnea and gall stone disease (USS abdomen)
- Endocrine diseases rarely cause obesity.
- Nonetheless, hypothyroidism, Cushing’s syndrome, hypothalamic tumors, and damage to the hypothalamus as a consequence of radiation, infection or trauma have all been associated with weight gain. These should be considered when indicated by patient history.
- Certain medications can contribute to obesity- steroids, antidepressants, sulphonylureas etc. Drug-induced effects should be suspected when the weight gain coincides with the initiation of the drug.
How do you treat obesity?
Treatment of obesity consists of several therapeutic options
- Life style changes- decrease energy intake and increase physical activity.
- This should be a component of all other therapies.
- Pharmacotherapy
- Bariatric surgery
What are the principles of weight loss programme?
- Based on balanced healthy diet
- Regular physical activity
- Weight loss of 0.5-1 kg a week
- Aim to lose 5-10% of body weight
Programme that do not meet these criteria are unlikely to help people maintain a healthy weight in the long term.
Waist should be measured at the Midpoint between the lowest rib and the iliac crest (WHO) at the end of expiration
How do you decide on the level of intervention?
The level of intervention should be based as follows
| BMI Classification |
Waist circumference | Comorbidities present |
||
|---|---|---|---|---|
| Low | High | Very high | ||
| Overweight | Advice on healthy weight & life style | Diet +Physical activity | Diet +Physical activity | Diet +Physical activity: consider drugs |
| Obesity I | Diet +Physical activity | Diet +Physical activity | Diet +Physical activity | Diet +Physical activity: consider drugs |
| Obesity II | Diet +Physical activity: consider drugs | Diet +Physical activity: consider drugs | Diet +Physical activity: consider drugs | Diet +Physical activity: consider drugs: consider surgery |
| Obesity III | Diet +Physical activity: consider drugs: consider surgery | Diet +Physical activity: consider drugs: consider surgery | Diet +Physical activity: consider drugs: consider surgery | Diet +Physical activity: consider drugs: consider surgery |
NB- Comorbidities include T2DM, hypertension, cardiovascular disease, osteoarthritis, dyslipidaemia and sleep apnoea.
Discuss life style changes?
- Physical activity
- At least 30 minutes of moderate-intensity physical activity on 5 or more days a week. The activity can be in one session or several lasting 10 minutes or more.
- Diet
- 600 kcal/day deficit diet (that is, they contain 600 kcal less than the person needs to stay the same weight) are recommended for sustainable weight loss.
- Low-calorie diets (1000–1600 kcal/day) may be considered, but are less likely to be nutritionally complete.
- Very-low-calorie diets (less than 1000 kcal/day) may be used for a maximum of 12 weeks continuously, or intermittently with a low-calorie diet (for example for 2–4 days a week), by people who are obese and have reached a plateau in weight loss.
Discuss Pharmacological interventions?
Drug treatment should be considered for patients who have not reached their target
weight loss or have reached a plateau on life style changes. Drug treatment is not
generally recommended for children younger than 12 years.
- Orlistat (Xenical)
- Mechanism- Peripheral lipase inhibitor; causes fat malabsorption.
- Side effects- Fatty stool, Urgency, possible vitamin malabsorption
- Mean weight loss- 2.9 kg (2.3-3.4)
- Standard prescription dose of 120 mg three times daily before meals
- The co prescribing of Orlistat with other weight loss drugs is not recommended.
- Sibutramine (Meridia in the U.S. and Canada, Reductil in Europe)
- It is a SNRI (serotonin & norepinephrine reuptake inhibitor). It induces satiety
- Side effects- Insomnia, Dry mouth, Nausea, Constipation, Increased blood pressure & heart rate. Pulse & blood pressure should be specifically monitored.
- Mean weight loss- 4.6 kg (3.8-5.4)
- 10 mg once daily (usually in the morning), if this proves insufficient the dose may be increased to 15 mg daily after 4 weeks.
- Contra indication. Patients with uncontrolled hypertension, IHD, arrhythmias, congestive heart failure, stroke or transient ischemic attacks, seizure disorder, or severe kidney or liver disease.
- Co prescribing of Sibutramine with other wt loss drugs is not recommended.
- Rimonabant (Acomplia, withdrawn from UK)
- Selective cannabinoid-1 receptor (CB1) blocker. Blocking CB1 receptors reduces over activity of the endocannabinoid system (ECS). This contributes to the regulation of energy homeostasis and improves lipid profile, components of the metabolic syndrome, and glucose uptake.
- Mean weight loss- 4.6 kg (4.3-5.0)
- Side effects- Nausea, Dizziness, Diarrhea, Insomnia, Depression
How do you decide which pharmacological intervention to use?
Sibutramine may be preferred in patients having difficulty controlling portion sizes due to hunger or not feeling full. It may also be useful in gastrointestinal conditions such as irritable bowel syndrome that would make it difficult to take orlistat.
Orlistat may be useful in patients needing additional motivation to adhere to a fat-modified diet
How long can you continue the drugs?
Discontinue if no response after 3 months (wt loss of at least 5%)
The medication may be continued if weight is lost within 6 months and is maintained after the initial weight loss phase. It can be continued as long as the patient continues to maintain weight loss and there are no significant adverse effects.
When would you recommend bariatric surgery?
Bariatric surgery is recommended as a treatment option for people with obesity if
all of the following criteria are fulfilled:
- They have a BMI of 40 kg/m2 or more, or between 35 kg/m2 and 40 kg/m2 and
- other significant co morbid diseases (like t2dm or hypertension) that could be
- improved if they lost wt.
- All appropriate non-surgical measures have been tried but have failed to
- achieve or maintain adequate, clinically beneficial weight loss for at least 6 m
- The person has been receiving or will receive intensive management in a Specialist obesity service
- The person is generally fit for anaesthesia and surgery
- The person commits to the need for long-term follow-up.
Remember
- Bariatric surgery is also recommended as a first-line option (instead of lifestyle
- interventions or drug treatment) for adults with a BMI of more than 50 kg/m2 in whom surgical intervention is considered appropriate.
- Surgery should be undertaken only after a comprehensive preoperative assessment of any psychological or clinical factors that may affect adherence to
- post operative care requirements, such as changes to diet.
What are the principles of bariatric surgery?
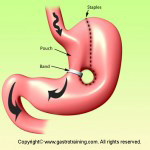
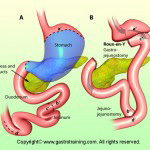
Two main principles exist in combination or alone: restriction and malabsorption.
Purely restrictive operations limit the amount of solid food that can be consumed.
NB- Biliopancreatic diversion with or without duodenal switch is another restrictive plus malabsorptive surgery. This is technically demanding and rarely performed.
Discuss post-operative complications of bariatric surgery? (Steinbrook R. NEJM 2004)
Combined Gastric Restriction & Malabsorption Operative Risks: (vs. cholecystectomy)
Perioperative Mortality 1-2% vs. 0.2-0.8%
Early Complications 10% vs. 2.9%
Late Complications 20% vs. 1-2%
| Early Complications (within 30 days) | Late complications |
|---|---|
| Mortality- 1% (in bypass surgery- 75% of all deaths are due to anastomotic leaks and 25 % are due to PE’s.) Anastomotic leak- 1.5% Pulmonary embolism- 2% Pneumonia- 1.9% Wound infection- 6% Acute gastric distension- rare |
Stomal Stenosis-3-20% (can be dilated upto 12mm with TTS balloon) Anastomotic Ulceration -3-20% Staple line disruption-1% Internal Hernia- rare Incisional Hernia- 15% Fistula-rare |
How do you monitor postoperatively?
There is a risk of nutritional deficiencies with malabsorptive operations.
Vitamin deficiencies- Thiamine, B12, folate, fat soluble vitamins, vitamin C
Minerals- Iron, calcium, zinc, selenium, copper
Deficiencies of protein and albumin could occur too.
There is lack of guidance regarding follow up and monitoring. However, it is suggested that;
FBC, urea and electrolytes, Ca, Mg, PO4, Glucose, LFTs, Ferritin, Vitamin B12, Folate, selenium, zinc, copper and fat soluble vitamins should be monitored at least 2-3 times a year
Bone mineral density should also be monitored
Lifelong supplementation of multivitamin tablets (including Lap band patients)
Ref