Use of IV Ciclosporin in the Treatment of Refractory Acute Severe UC in Adults
Discuss severe UC?
- Severe UC is a potentially life threatening condition.
- 65% of patients treated with corticosteroids will be symptom free by the end of five days, 15% will have significant improvement, and 25% will not improve. Those who fail to improve may be treated with intravenous ciclosporin or undergo colectomy.
- The mortality in severe UC is currently < 1% in specialist centres.
- Thus only one patient in a hospital need to die from delayed decision making or complications of ciclosporin to negate the benefit of medical therapy. Ultimately it is about saving lives, not colon.
Define severe acute UC?
Severe acute UC is usually defined by the original classification put forward by Truelove and Witts. They defined severe UC as presence of six or more bowel motions per day associated with one or more of the following:
- temperature >37.8
- Large amounts of rectal bleeding
- Heart rate >90/minute
- Haemoglobin of <10.5 g/dl
- ESR >30 mm/h
Can you predict the need for surgery in severe acute UC?
- A delay in referral for colectomy is associated with increased mortality. It is thus clearly important to identify those who are likely to need colectomy at an early stage, so that surgery is not inappropriately delayed.
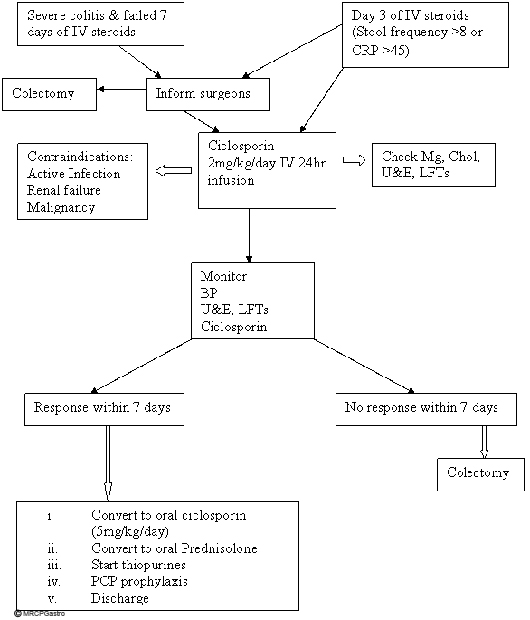
- The simplest approach is objective re-evaluation on the third day of intensive treatment. A stool frequency of more than 8/day or CRP of > 45mg/L at 3 days predicts the need for colectomy on that admission in 85% of cases.
- It must be understood that the CRP and stool frequency criteria are simply a guide and neither immutable nor always reproduced. However, at the very least, patients meeting these criteria may be considered for surgical referral and/or treatment with ciclosporin.
Discuss ciclosporin vs. infliximab in severe acute colitis?
- Response rates in controlled trials with infliximab in corticosteroid-refractory UC patients are inferior to those reported with intravenous ciclosporin therapy, although the two drugs have not been compared directly.
- It is worth noting that most intravenous cyclosporine trials report 60 to 85 percent response rates in corticosteroid-resistant UC.
- Currently, infliximab can be considered in patients with acute steroid-refractory disease who are reluctant to undergo colectomy and in whom ciclosporin is contraindicated
Discuss the evidence for ciclosporin use in severe acute UC?
- There have been four controlled studies of intravenous ciclosporin in patients with severe ulcerative colitis.
- These trials showed that intravenous ciclosporin (with continued IV steroids) is effective in inducing remission in more than 80% of patients with severe ulcerative colitis.
- An initial dose of 2mg/kg/day intravenous ciclosporin is as effective as 4mg/kg/day and is thus preferred from the standpoint of safety.
- However, the long-term outcome of patients who have had their colon salvaged with ciclosporin is less promising. A series from Oxford reported that only 58% needed colectomy after 7 years follow up. Bojic reported that by failing corticosteroids the patient’s likelihood of requiring a colectomy in the next 10 years is 80%, regardless of the treatment.
Discuss the role of immunomodulators in decision making?
- The rate of colectomy was significantly higher in patients already taking azathioprine when ciclosporin was started compared with those who started azathioprine concurrently with ciclosporin.
- Ciclosporin is thus, at best, a bridge to maintenance therapy, and its use should be carefully considered if maintenance therapy with azathioprine or mercaptopurine is not an option, either because of intolerance to or relapse in spite of thiopurine therapy.
Who to treat with ciclosporin?
- Rescue therapy with ciclosporin could be considered on the third day of intensive treatment if predictive factors are poor (>8 bloody stools, or 3-8 bloody stools and CRP>45).
- Ciclosporin is suitable for patients with persistent severe colitis after 7 days of intravenous steroids who do not need immediate colectomy.
- Use of ciclosporin should be carefully considered in the following cases:
- Long standing chronic active colitis
- Pancolitis for >10 years
- Thiopurine resistance or intolerance
- Do not use ciclosporin in presence of moderate to severe renal impairment (creatinine > 130 micromol/litre or 20-30% reduction in eGFR), previous or current malignancy (except treated basal or squamous cell carcinoma) and current infection.
How to treat?
- 2 mg/kg/day as a 24 hr continuous IV infusion (continue up to 7 days depending on the response).
- Prerequisites before using ciclosporin:
- Check the renal function, LFTs, magnesium and cholesterol.
- Magnesium and cholesterol are best checked on admission in case intravenous ciclosporin is given.
- The risk of seizures is increased in patients with a low cholesterol (<3.0 mmol/l) or magnesium (<0.50 mmol/l). Oral therapy is an alternative in these circumstances. Microemulsion ciclosporin does not contain the chromophore present in intravenous ciclosporin that has been associated with neurotoxicity causing seizures in patients with hypocholesterolaemia or hypomagnesaemia.
- CMV colitis can mimic UC and is thought to be responsible for treatment failure in up to 10% of patients labelled as steroid refractory. Treatment of CMV may obviate colectomy. So consider doing a flexible sigmoidoscopy before starting ciclosporin.
- Monitoring
- Check ciclosporin levels on day 2 and then every 3 days (aim 100-200 ng/ml).
- Monitor U&E, LFT, Mg and Cholesterol on alternate days.
- Reduce the ciclosporin dose by 25% if any of these occur:
- serum creatinine rises by more than 30% from baseline
- SBP is > 150mm Hg or DBP exceeds 90 mm Hg despite antihypertensive treatment. Hypertension is treated with a calcium channel blocker such as nifedepine, because it may offer protection against ciclosporin induced nephrotoxicity. However the use of calcium channel blockers can lead to a rise in serum ciclosporin levels, so careful drug level monitoring is essential.
- Serum liver enzymes double
When to convert to oral ciclosporin?
- Once response occurs convert to oral ciclosporin in 2 divided doses. An oral dose of 5mg/kg/day is equivalent to 2mg/kg/day intravenous dose since the oral bioavailability of neoral is 30-40%. However the blood levels need to be monitored and the dose titrated accordingly.
- Convert to oral steroids at the same time and taper dose by 5mg every week.
- Consider starting (or optimizing to maximum dose if already on thiopurines) azathioprine or mercaptopurine before discharge.
- The patient may be discharged home after 1-2 days of observation on oral ciclosporin.
- Measure ciclosporin levels at week 1 and week 2 and then monthly.
- Use PCP prophylaxis with triple immunosuppression (Co-trimoxazole 960mg 1 tab administered three times per week).
When do you consider stopping ciclosporin?
Discontinue ciclosporin after 3-6 months by reducing the dose by 50% for 2 weeks, followed by complete ciclosporin withdrawal.
What is the bottom line for ciclosporin?
By careful selection of patients at high risk of colectomy, (avoiding those in poor general condition), and use of low-dose i.v or oral ciclosporin at an early stage, ciclosporin is a safe and effective salvage therapy in acute colitis. With the introduction of thiopurines on discharge from hospital and continuing ciclosporin for 3-6 months, long term results could be maximized, with about 40-50% long term success.
Discuss measurement of ciclosporin levels?
The levels could be done at anytime during the 24 hr infusion. Trough levels are needed once the patient is on oral ciclosporin.
Ref
- Stenner JMC, White P, Gould SR. Audit of the management of severe ulcerative colitis in a DGH. Gut 2001; 48:A87.
- Travis SPL, Farrant JM et al. Predicting outcome in severe ulcerative colitis. Gut 1996; 38:905-10.
- Ho GT, Mowat C, Goddard C. Predicting outcome and risk assessment in severe ulcerative colitis. Gastroenterology 2003; 124:A2.
- Lichtiger S, Present, DH, Kornbluth, A, et al. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med 1994; 330:1841-5
- D’Haens G, Lemmens L, Hiele M, et al. Intravenous corticosteroids as single therapy for severe attacks of ulcerative colitis. Gastroenterology 2001; 120:1323-9.
- Svanoni F, Bonassi U, Bagnolo F, et al. Effectiveness of cyclosporine A (CsA) in the treatment of active refractory ulcerative colitis (UC). Gastroenterology 1998; 114:A1096.
- Van Assche G, D’Haens, G, Noman, M, et al. Randomized, double-blind comparison of 4 mg/kg versus 2 mg/kg intravenous cyclosporine in severe ulcerative colitis. Gastroenterology 2003; 125:1025-31.
- Campbell S, Travis S, Jewell D. Ciclosporin use in acute ulcerative colitis: a long term experience. Eur J Gastroenterol Hepatol 2005; 17:79-84.
- Bojic D, Al-Ali M, Jewell DP et al. Pattern and outcome of severe ulcerative colitis 2005, 15 year data. Gut 2005:54(suppl. VII):A155.
- Cohen RD, Brodsky AL, Hanauer SB. A comparison of the quality of life in patients with severe ulcerative colitis after total colectomy versus medical treatment with intravenous cyclosporin. Inflamm Bowel Dis 1999; 5:1-10.
- Carter MJ, Lobo AJ, Travis SP .Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004 Sep; 53 Suppl 5:V1-16.
- Cottone M, Pietrosi G, Martorana G et al. Prevalence of cytomegalovirus infection in severe refractory ulcerative and Crohn’s colitis. Am J Gastroenterol 2001; 96:773.
- Morales JM, Andres A et al. Calcium antagonist therapy prevent chronic cyclosporin nephrotoxicity after renal transplantation. Transplant Proc 1992;24:89-91
- Actis GC, Volpes R, Rizzetto M. Oral microemulsion cyclosporin to reduce steroids rapidly in chronic active ulcerative colitis. Eur J Gastroenterol Hepatol 1999; 11: 905–8.