Gastric cancer
Discuss the changing pattern of gastric cancer?
The incidence of cancer of the cardia and gastroesophageal junction has been rapidly rising whereas cancer of the distal half of the stomach has declined rapidly over the recent few decades.
What are the risk factors for gastric cancer?
Helicobacter pylori infection, older age, male gender, diet including dry salted foods, atrophic gastritis, pernicious anemia, cigarette smoking, Menetrier’s disease, and familial polyposis
Discuss the pathogenesis of gastric cancer?
A widely accepted model of gastric cancer describes a progression from chronic gastritis to chronic atrophic gastritis, to intestinal metaplasia, dysplasia, and eventually to adenocarcinoma. The following steps are described:
- Longstanding chronic superficial gastritis caused by chronic H. pylori infection leads to chronic atrophic gastritis and intestinal metaplasia.
- Gastric atrophy leads to loss of parietal cell mass and consequent hypochlorhydria. This causes increase in serum gastrin, a potent inducer of gastric epithelial cell proliferation.
- The increase in gastric pH permits colonization of bacteria capable of converting dietary nitrates to potent mutagenic N-nitroso compounds.
- Chronic inflammation also results in epithelial cell damage with increased free radical generation and increased cell turnover.
Hypochlorhydria due to gastric resection or autoimmune pernicious anemia will lead to similar chain of events.
Is Intestinal metaplasia (IM) reversible?
IM is a potentially reversible change. It occurs as a result of Helicobacter pylori infection
or other environmental stimuli. Epidemiological studies have shown that intestinal metaplasia in the stomach have a high cancer risk.
What are the clinical features of gastric cancer?
- Weight loss and persistent abdominal pain are the most common symptoms at initial diagnosis.
- Dysphagia in cancers arising in the gastric cardia or at the OG junction.
- Nausea or early satiety from gastric outlet obstruction or gastric stasis related to tumor infiltration of the stomach wall.
- Occult GI bleeding with or without iron deficiency anemia is common, while overt bleeding (ie, melaena or haematemesis) is seen infrequently.
How do you diagnose gastric cancer?
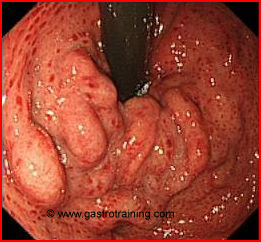
- Endoscopy and biopsies- The diagnosis of diffuse-type gastric cancer, so called “linitis plastica,” can be difficult as it may be associated with a relatively normal endoscopic appearance. Further these tumors tend to infiltrate the submucosa and hence superficial mucosal biopsies may be falsely negative.
- CT scan of chest/abdomen/pelvis to stage the disease.
- EUS is better than CT at assessing tumor depth (T stage) and perhaps lymph node involvement (N stage).
- PET-CT- The role of PET- CT in the staging of oesophago-gastric cancers is under evaluation. It is now increasingly being used in all cases of fit patients with an oesophageal or oesophago-gastric junction cancer which is suitable for radical treatment to detect occult stage IV disease.
- Laparoscopy is routinely used following CT and EUS in patients with T2 or greater gastric cancer prior to radical treatment. It is also considered in any patients where there is suspicion of peritoneal spread on CT or EUS such as in the presence of small volume ascites.
- Bone scan- Patients with advanced disease (>T2N0) who have not undergone full body PET-CT require a bone scan to exclude bony metastases.
Discuss TNM staging for gastric cancer?
T1- Tumor invades lamina propria or submucosa
T2- Tumor invades muscularis propria or subserosa
T3- Tumor penetrates serosa without invasion of adjacent structures.
T4- Tumour invades adjacent structures.
N1- Metastasis in 1 to 6 regional lymph nodes.
N2- Metastasis in 7 to 15 regional lymph nodes.
N3- Metastasis in more than 15 regional lymph nodes.
M0- No distant metastasis
M1- Distant metastasis.
Stage IA- T1N0M0, IB- T1N1M0/T2N0M0
Stage II- T1N2M0 /T2N1M0/T3N0M0
Stage III- T2N2M0/ T3N1-2M0/T4N0M0
Stage IV- Any N3 or M0 or T4N1M0
NB- The regional lymph nodes are the perigastric nodes, found along the lesser and greater curvatures, and the nodes located along the left gastric, common hepatic, splenic, and coeliac arteries. Involvement of other intra-abdominal lymph nodes, such as the hepatoduodenal, retropancreatic, mesenteric, and para-aortic, is classified as distant metastasis.
Discuss the management of gastric cancer?
How do you define a resectable gastric cancer?
- Surgical resection including regional lymphadenectomy is the treatment of choice for patients with stage I and II gastric cancer
- Stage III- All newly diagnosed patients with stage III gastric cancer should be considered candidates for clinical trials. However, Up to 15% of selected stage III patients can be cured by surgery alone, particularly if lymph node involvement is minimal (<7 lymph nodes). So, all patients with tumors that can be resected should undergo surgery.
- In practice, curative resectional procedures are confined to patients who at the time of surgical exploration do not have extensive nodal involvement.
What is the type of surgery undertaken?
- Total gastrectomy is usually performed for lesions in the upper third of the stomach and subtotal gastrectomy for lesions in the lower two-thirds. The mortality of total gastrectomy is approximately twice that of a subtotal gastrectomy.
- Regional lymphadenectomy is undertaken with both total and sub total gastrectomy. Splenectomy is not routinely performed.
- EMR may be considered as a definite treatment option in Early Gastric Cancer (adenocarcinoma limited to the gastric mucosa and submucosa). H.Pylori should be eradicated in patients with early gastric cancer.
What is the role of chemoradiotherapy?
- Neoadjuvant chemotherapy remains investigational with no definite evidence of survival benefit and clinical trials are continuing. However, the UK MRC ST02 MAGIC trial reported a significant 5 year survival advantage for those patients receiving 3 courses of neoadjuvant ECF chemotherapy. These patients had a 5 year survival of 36% compared to 26% for those patients having surgery alone. Following the publication of this trial, a number of cancer centers offer neoadjuvant ECF chemotherapy to all suitable patients.
- Adjuvant chemotherapy/chemoradiotherapy is currently not standard practice for resected gastric cancer. However, the impressive result of the well conducted MAGIC trial is leading to the adoption of the adjuvant chemotherapy approach in much of Europe and other parts of the world.
Discuss unresectable or metastatic disease?
What is unresectable disease?
Any T4 lesion
Any N3 lesion
Any M lesion
What are the treatment options for unresectable gastric cancer?
- Chemotherapy is the usual treatment. It provides quality of life and survival benefit. The combination of epirubicin, cisplatin, and continuous infusion of 5-FU (ECF) appears to be one of the most active regimens.
- While chemotherapy is the most effective treatment modality for metastatic disease, it is often less successful for control of symptoms related to local tumor progression such as nausea, pain, obstruction, or bleeding. Palliative resection may be needed for patients with continued bleeding or obstruction. Palliative radiation therapy may also alleviate bleeding, pain, and obstruction.
- Endoscopic destruction (APC/Laser) of obstruction of the gastric cardia is very helpful to patients whose tumors have occluded the gastric inlet.
How do you treat recurrent gastric cancer?
Curative resection is not possible in patients with recurrent disease. Most such patients require will systemic chemotherapy or palliative RT.
What is the prognosis?
5 year survival rates;
IA — 78 percent IB — 58 percent
II — 34 percent
IIIA — 20 percent IIIB — 8 percent IV — 7 percent
What is the criterion for the diagnosis of familial gastric cancer?
What is familial gastric cancer?
Consensus criteria for the diagnosis of familial gastric cancer have been proposed by the International Gastric Cancer Linkage Consortium (IGCLC);
i. 2 cases of diffuse type gastric cancer in 1st/2nd degree relatives with one <50 years old OR
ii. 3 cases of diffuse type gastric cancer in 1st/2nd degree relatives of any age
Genetic testing is recommended to patients who fulfill the IGCLC criteria above, or those whose family history also includes other malignancies potentially related to E-cadherin gene CDH1 mutations including lobular breast cancer or signet ring cancer of the colon.
What is the role of primary prevention in gastric cancer?
- H.Pylori eradication is a potential strategy in the primary prevention of gastric cancer. Whether H. pylori eradication therapy can reverse or reduce the risk that precursor lesions (gastric atrophy, intestinal metaplasia, or gastric dysplasia) will progress is controversial. However, current data do suggest a role for screening and eradication strategies at least in some settings.
- Screening for H. pylori is not currently recommended in areas with a low-incidence of gastric cancer (UK) but it is reasonable to screen patients who have risk factors (previous gastrectomy, pernicious anemia, family history) for gastric cancer regardless of the baseline risk in the population.
Ref